
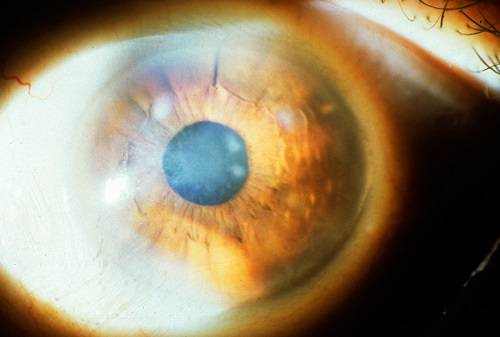
At 2020 Eyecare Ohio, we offer scleral lenses as a keratoconus treatment option. With more severe keratoconus, an optometrist may recommend hard contact lenses. This treatment is the same solution used for patients with myopia (nearsightedness) and astigmatism. This is typically when a patient is in their teens or early 20s. In the early stages, keratoconus can be treated with prescription eyewear. Treatments for keratoconus depend on a patient’s age and the severity of the condition. Additionally, a history of asthma, allergies, Ehlos Danlers syndrome, Down’s syndrome, or retinitis pigmentosa can put a person at risk for developing keratoconus. In the United States, 1 in 10 patients with keratoconus has a close relative with the disorder, too. The exact causes of keratoconus aren’t certain, but research shows that significant factors could include: While keratoconus is a less common eye condition, it can become a more serious issue if left untreated. With time, more symptoms can develop, such as: Generally, the early stages of keratoconus are characterized by slight blurring or distortion in a person’s vision and frequent changes to glasses prescription- like every few months. The symptoms of keratoconus can change or worsen with time as the condition progresses. While there is no known way to prevent keratoconus, several treatments are available to help people with this condition see clearly and comfortably. These cracks can take weeks or months to heal, but your optometrist can prescribe eye drops to help you recover. This swelling occurs when the strain of the corneal bulging creates small cracks along the back surface. In rare cases, the cornea can swell and cause significant vision impairment. This condition can continue to progress until a person is in their mid-30s, or longer, depending on the person.Īs keratoconus progresses, the cornea bulges out further (creating that cone shape) and causing more vision issues. Keratoconus affects approximately 1 in every 2,000 people and usually first presents during puberty. Pachymetry: measurement of the thinnest parts of the cornea.Slit-lamp exam: corneal exam to check for abnormalities.Corneal topography: digital imaging used to map the cornea’s curvature.To diagnose keratoconus, your optometrist will review your medical history and complete a comprehensive eye exam. The irregular shape prevents the proper focusing of light once it enters the eye, causing vision issues. Often, their cornea becomes more cone-shaped. Patients who have keratoconus have a thin, misshapen cornea. No matter how you turn it, the curve and shape should remain the same. Typically, the cornea (clear front surface of the eye) is a round, dome shaped surface. Keratoconus is an eye condition that results in an irregularly shaped cornea. Keratoconus is a less common condition, but can have a serious impact on a person’s vision.

However, there are many conditions that can impact our vision. The eye has special muscles that are always adjusting to changes in our environment, protecting our ability to see, and working hard to ensure we can see clearly.


 0 kommentar(er)
0 kommentar(er)
